Algorithm based approach to pre-emptive liver and liver- kidney transplantation in children with Primary Hyperoxalosis type-1
Jagadeesh Menon1, Naresh Shanmugam1, Ravikumar Thambidurai2, Chandrasekaran Venkataraman3, Ashwin Rammohan4, Gomathy Narasimhan4, Akhila Rajakumar5, Ilankumaran Kaliamoorthy5, Mohamed Rela4.
1Pediatric gastroenterology and hepatology , Dr Rela Institute & Medical Centre, Chennai, India; 2Pediatric intensive care, Dr Rela Institute & Medical Centre, Chennai, India; 3Pediatric nephrology, Dr Rela Institute & Medical Centre, Chennai, India; 4Hepatobiliary surgery & liver transplantation, Dr Rela Institute & Medical Centre, Chennai, India; 5Liver anesthesia and intensive care, Dr Rela Institute & Medical Centre, Chennai, India
Background: Primary hyperoxalosis type-1 (PH-1) is an important cause of chronic kidney disease (CKD) in children. A liver transplant(LT) with or without kidney transplant(KT) is the only available cure for PH-1.
Method: A retrospective analysis was performed on patients undergoing pre-emptive liver(pLT), simultaneous (SimLKT) or sequential liver and kidney(SeqLKT) transplant for PH-1 from Jan 2011 to September 2024 at our institute. Clinical profile, details of LT and/or KT, post-transplant complications, graft and patients survival between groups were analysed.A management algorithm was subsequently proposed (Fig1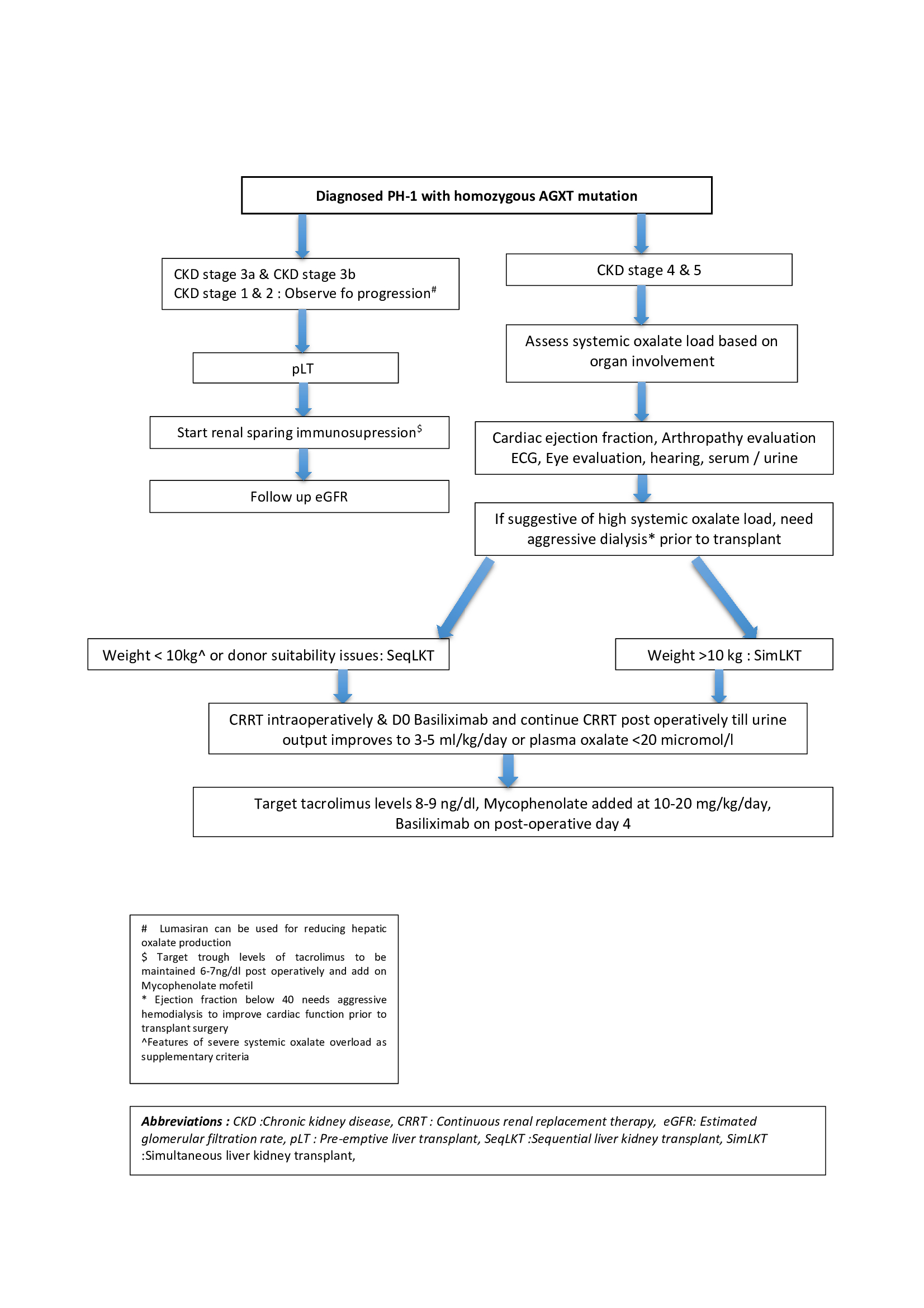 ).
).
Result : Of 787 pediatric LT in the aforementioned time period, 28 (3.5%) were performed in children with PH-1(20 males &10 females). This included pLT 6 (20%), simultaneous liver kidney (SimLKT) 13 (50%), and 9 (30%) sequential liver kidney transplantation (SeqLKT). Twenty two (80%) had a pre-transplant dialysis; peritoneal 12 (52%) and hemo-dialysis 10 (48%). Median age of LT was 60 (12-108), 108 (48-264), 72 (6-168) months in pLT, SimLKT and SeqLKT respectively. Living donor transplants were 27(96%). No children had rejection, vascular or biliary issues in post LT period. After a median follow up of 60 months, 75% patients are alive with highest mortality in SeqLKT group (Fig 2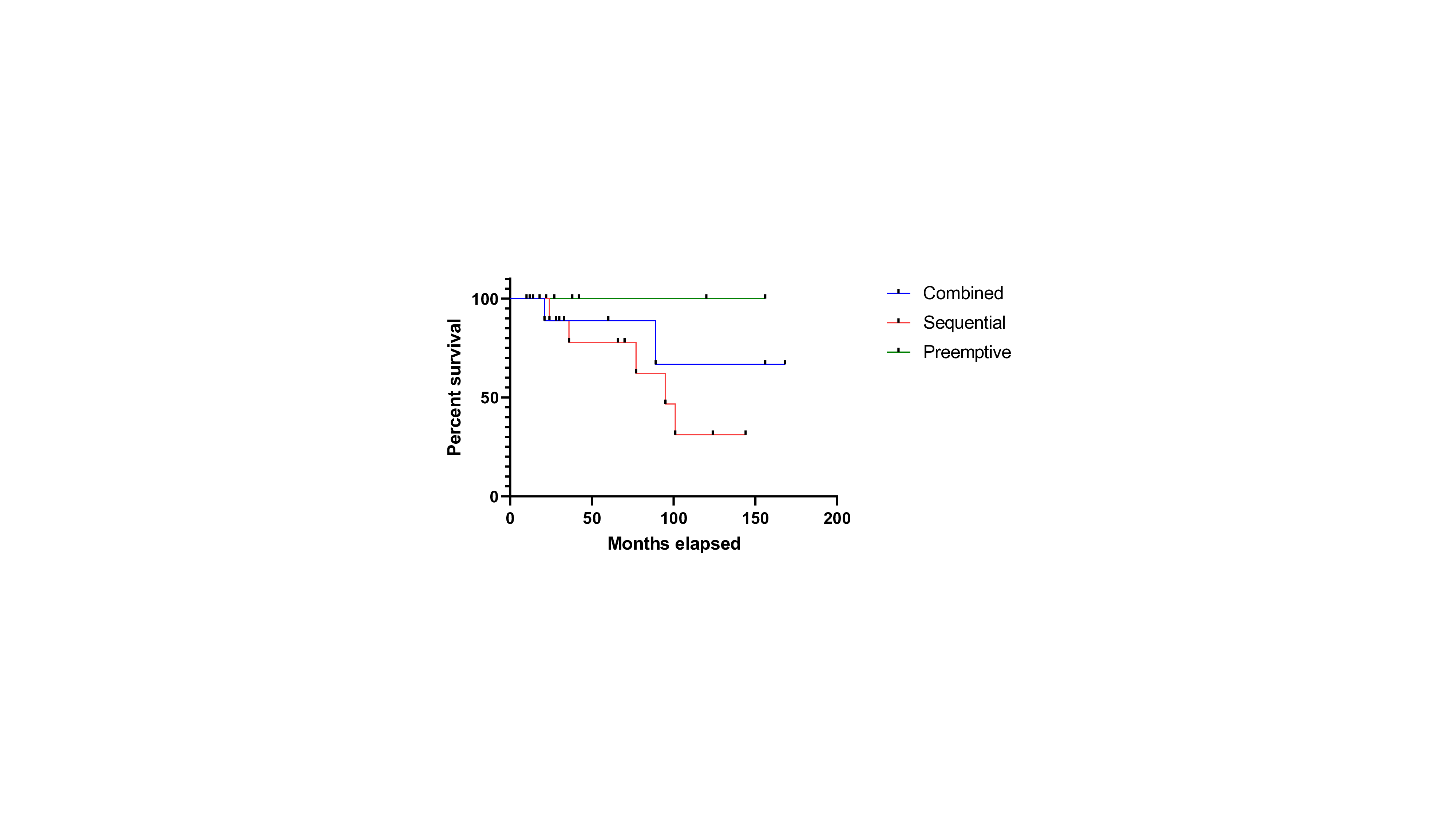 ). Renal functions were stable in pLT group after a median follow up of 40 (22-156) months. None had graft dysfunction of either liver or kidney in the SimLKT group.
). Renal functions were stable in pLT group after a median follow up of 40 (22-156) months. None had graft dysfunction of either liver or kidney in the SimLKT group.
Conclusion : A SimLKT should be the preferred treatment modality in patients with PH-1 having end stage kidney disease. A pLT in those patients with early renal involvement prevents further disease progression.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00