The Society of Pediatric Liver Transplantation (SPLIT): 2023 Registry Status
Anna Banc-Husu1, Rachel Smith2, Beau Kelly3, Ravinder Anand4, Sarah Anderson4, Steve Lobritto5, Evelyn Hsu6, James E Squires2, Pamela L Valentino6.
1Division of Gastroenterology, Hepatology, and Nutrition; Department of Pediatrics, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States; 2Division of Gastroenterology, Hepatology, and Nutrition; Department of Pediatrics, UPMC Children’s Hospital of Pittsburgh, Pittsburgh, PA, United States; 3DCI Donor Services, Sarcamento, CA, United States; 4Emmes Corporation, Rockville, MD, United States; 5Division of Gastroenterology, Hepatology, and Nutrition; Department of Pediatrics and Medicine, Columbia University Irving Medical Center, New York City, NY, United States; 6Division of Gastroenterology and Hepatology, Department of Pediatrics, Seattle Children’s Hospital, University of Washington School of Medicine, Seattle, WA, United States
Background: The Society of Pediatric Liver Transplantation (SPLIT) has undergone tremendous growth with >45 sites contributing data focusing on improving outcomes in pediatric liver transplantation (LT). We report and compare outcomes from the SPLIT Registry.
Methods: Patients <18 years with first-time LT only enrolled into the SPLIT Registry between 2011-2023 were included. Data was stratified into eras from last published registry update (era 1: 2011-2018, era 2: 2018-2023).
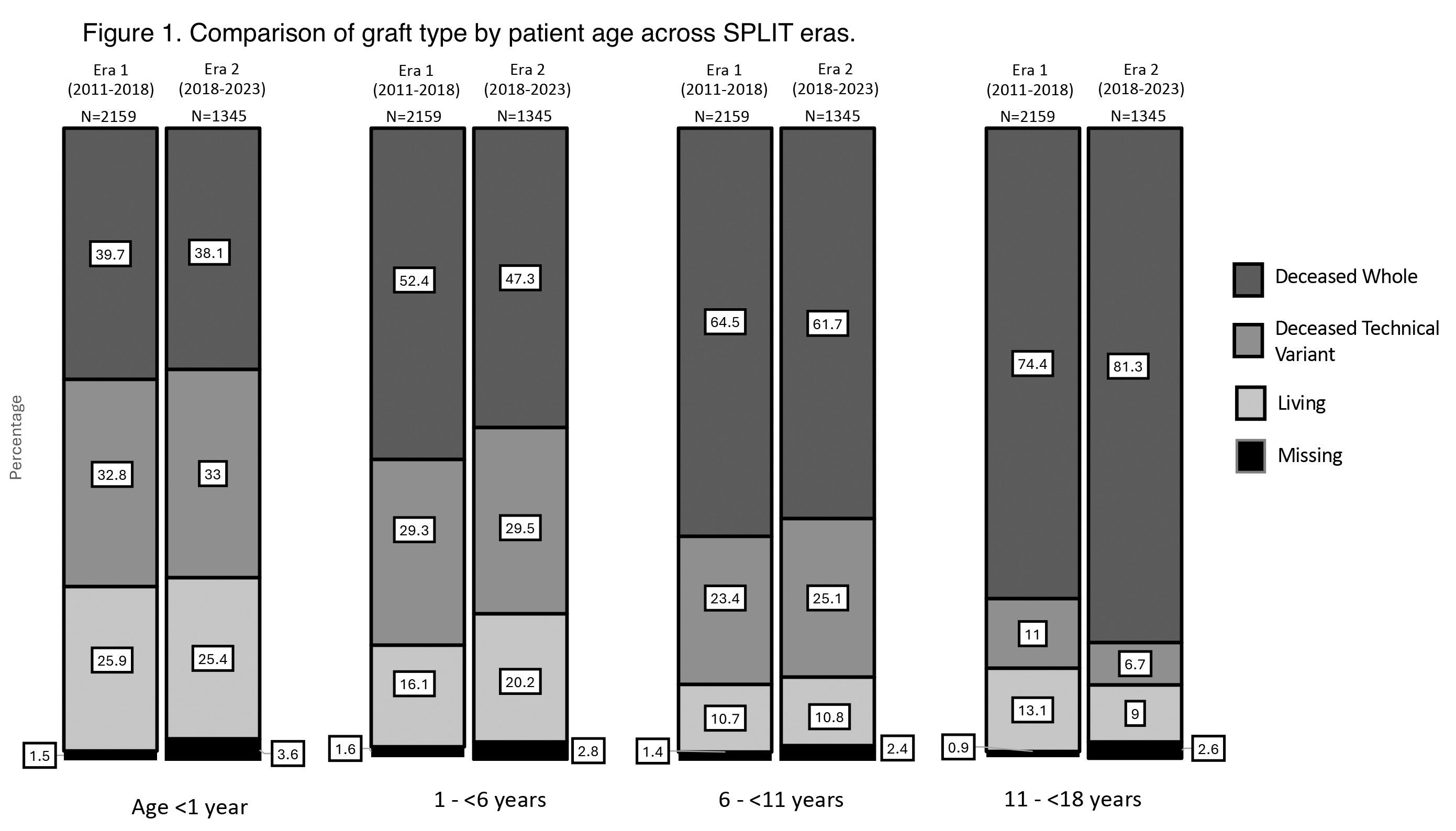
Results: 3,504 participants from 47 centers were included (era 1: n=2,159; era 2: n=1,345). Age distribution differed with more children <1 yr of age at LT in era 2 (era 1: 29% vs. era 2: 33%, p=0.01). Indications for LT were similar, with biliary atresia (38.8%) and metabolic disease (16.0%) being most common. Exception point use was higher in era 2 (era 1: 45% vs. era 2: 56%, p<0.001). No difference in graft type (deceased: 81% era 1 vs. 78% era 2, p=0.78), patient survival at 90 days (era 1: 98.7% vs. era 2: 98.3%), 1 year (era 1: 97.2 vs era 2: 96.8%), or 3 years (era 1: 95.3% vs. era 2: 95.2%) were noted. Rate of hepatic artery thrombosis was lower in era 2 (era 1: 7% vs. era 2: 5%, p=0.02).
Conclusions: Trends in pediatric LT within SPLIT note similar LT indications and graft type, higher utilization of exception points, and lower HAT rates despite transplanting more children <10 kg. This data underscores the evolution of pediatric LT towards higher survivability and overall patient outcomes.
The authors would like to acknowledge the Society of Pediatric Liver Transplantation, the data contributions, proposal review, study design revision, and project oversight approval by SPLIT, Inc., the SPLIT Registry, and Emmes. Funding for data preparation and management was provided by SPLIT Inc. The data analysis, conclusions, and any recommendations in this body of work are supported by SPLIT..
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00