Acute-on-Chronic Liver Failure (ACLF) in children with cirrhosis is associated with worse post-transplant survival and increased resource utilization
Anna Banc-Husu1, Kathleen Hosek2, Matt Hall3, Divya Sabapathy4, Moreshwar Desai4, Fong W Lam4, Daniel H. Leung1, Benjamin L. Shneider1.
1Division of Gastroenterology and Hepatology, Department of Pediatricsterolo, Baylor College of Medicine, Texas Children's Hospital, Hosuton, TX, United States; 2Division of Critical Care, Department of Pediatrics, Baylor College of Medicine, Texas Children's Hospital, Houston, TX, United States; 3Division of Solid Transplant Surgery, Department of Surgery, Texas Children's Hospital, Houston, TX, United States; 4Children's Hospital Association, Lenexa, KS, United States
Background: The impact of ACLF on liver transplant (LT) outcomes in children with chronic liver disease (CLD) has not been well characterized. Current data are sporadic and limited to biliary atresia (BA) or single-centers. Our aim was to systematically characterize ACLF and determine its effect on post-LT outcomes and resource utilization in children with CLD.
Methods: Using linkage of the Scientific Registry of Transplant Recipients and billing data from Pediatric Health Information System (PHIS), we identified children with CLD between 3 months to <18 years at time of listing who received LT from 2002-2020. For this anaylsis, ACLF was defined by ≥ 1 extra-hepatic organ failure (OF) prior to LT: CV failure (pressors), respiratory failure (CPAP/BIPAP/ventilator), renal failure (renal replacement therapy), neurologic failure (ICD-9/10 hepatic encephalopathy). ACLF grade was defined by number of OFs with ACLF-1 = 1 OF, ACLF-2 = 2 OF, and ACLF-3 ≥ 3 OF. Resource utilization (including total billed charges) and donor/recipient characteristics were compared using Kruskal-Wallis and Chi-square. Kaplan-Meier was used for patient/graft survival analysis. Results depicted as median [p25-p75].
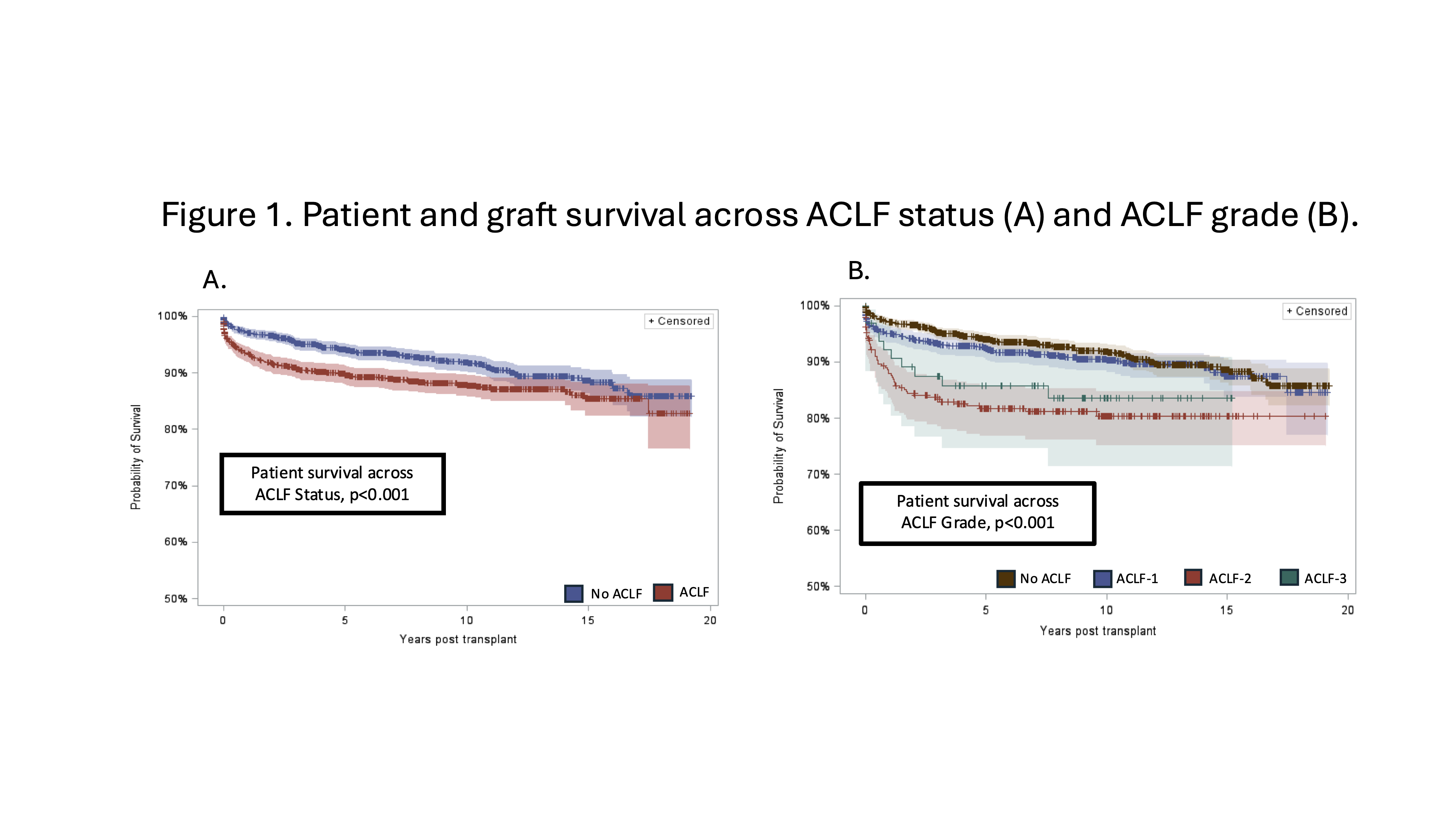
Results: A total of 3,003 patients (54% F) with CLD (56% cholestatic [last TBili ≥3.0], 22% biliary without cholestasis, 15% hepatocellular, 7% other), median age at listing of 1.1 years [0.5–7.7], and age at LT of 1.7 years [0.8–8.7] were included. There were 13,185 pre-LT and LT hospitalizations, with a total of 1,824 (14%) ACLF hospitalizations. 1,321 patients (44%) had ≥ 1 ACLF hospitalization, of which 73% (959/1321) had ACLF-1, 22% (296/1321) had ACLF-2, and 5% (66/1321) had ACLF-3. CV failure was most common (75%, n=1000) and renal failure was least (10%, n=130). ACLF was associated with longer waitlist times (97 days [37-215] vs. 81 [30-205], p=0.01), fewer living donor grafts (11% vs. 19%, p<0.001), and Status 1B listing (15% vs. 2%, p<0.001). Pre-LT resource utilization was higher in ACLF with longer overall LOS (9 days [4-17] vs. 3 [2-7], p<0.001), longer ICU LOS (3 days [2-6] vs. 2 [1-3], p<0.001), and higher total billed charges ($88,512 [$36,551-$191,289] vs. $24,134 [$11,795-$50,929], p<0.001). Similarly, ACLF had increased index LT hospitalization LOS (26 days [14-52] vs. No ACLF 18 [11-34], p<0.001), increased ICU LOS (8 days [4-20] vs. 5 [3-10], p<0.001), and total billed charges ($54,4677 [$313,711-$1,026,831] vs. $368,699 [$239,598-$587,113], p<0.001). Post-LT patient/graft survival was worse in patients with ACLF (Figure 1A), p<0.001, even when comparing across grade (Figure 1B, 1C), p<0.001.
Conclusion: This is the largest cohort describing the impact of ACLF on listing, graft use and post-LT outcomes in children with CLD. ACLF was associated with longer waitlist times and resource utilization was 3.6-fold and 1.5-fold higher in both pre-LT and index LT hospitalizations. Children who experienced pre-LT ACLF had overall worse post-LT survival.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00