From Invisible to Actionable: Clinical Use of PROMs in Pediatric Liver Transplantation
Karina Kwan1,2, Mar Miserachs1,2, Mary Flanagan1,2, Krista Van Roestel1,2, Maria De Angelis1,2, Tara McDonald1,2, Jennifer Stunguris1,2, Shira Segal1,2, Yaron Avitzur1,2, Vicky Lee Ng1,2.
1Division of Gastroenterology, Hepatology and Nutrition, The Hospital for Sick Children, University of Toronto, Toronto, ON, Canada; 2Transplant and Regenerative Medicine Centre, The Hospital for Sick Children, Toronto, ON, Canada
Introduction:
Patient-reported outcome measures (PROMs) provide a standardized way for patients to share insights on well-being, quality of life, mental health, treatment satisfaction, and future health goals—often “invisible” metrics until these issues escalate. Although PROM integration into post-pediatric LT (pLT) clinical care has demonstrated feasibility, sustained use has stalled. This study investigates the PeLTQL in identifying common patient-reported concerns in a representative cohort to aid intervention planning and resource allocation.
Methods:
PeLTQL data from patient-parent dyads completed between 01/01/2022 to 02/03/2025 were reviewed. Likert responses were converted to a 0–100 scale generating a total (PeLTQL-TS) and three subdomain scores: Future Health, Coping & Adjustment, and Social-Emotional. A PeLTQL-TS value < 62.5 indicates “at-risk” for anxiety.
Results:
A total of 161 PeLTQLs were identified; 83 completed for a research study and 2 with too many missing responses were excluded. The final cohort was comprised of 61 subjects completing 76 PeLTQLs, with 15 (25%) completing two (Table 1). 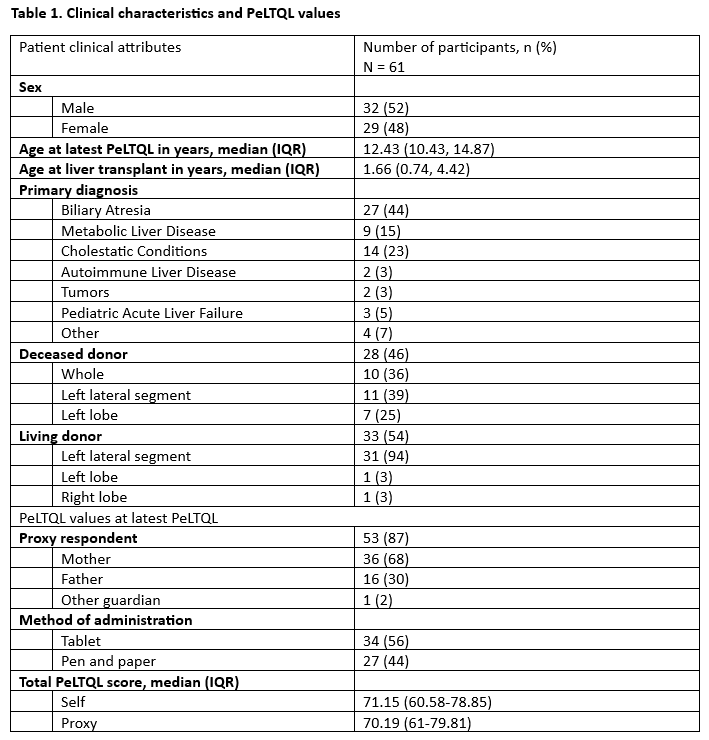 The intraclass correlation coefficient (ICC) was 0.54 (95% CI, 0.31-0.71), indicating moderate dyad agreement. The top self-reported concerns were scar visibility (26%) and overprotective parents (25%). Eighteen (32%) patients were identified as “at-risk” (median (IQR) self-PeLTQL-TS 55.29 (49.03-59.86)), whereas 62% of their parents reported “not at-risk” proxy-PeLTQL-TS scores (64.5 (55.05-75.24); p=0.03). “At-risk” patients were more likely than not “at-risk” patients to report concerns about scar visibility (62% vs 10%), future health problems (40% vs 2%), being treated differently (38% vs 2%), and overprotective parents (33% vs 14%). Eight (57%) of the patients who completed the PeLTQL twice reported a change in PeLTQL-TS exceeding the minimal clinically important difference of 6.45.
The intraclass correlation coefficient (ICC) was 0.54 (95% CI, 0.31-0.71), indicating moderate dyad agreement. The top self-reported concerns were scar visibility (26%) and overprotective parents (25%). Eighteen (32%) patients were identified as “at-risk” (median (IQR) self-PeLTQL-TS 55.29 (49.03-59.86)), whereas 62% of their parents reported “not at-risk” proxy-PeLTQL-TS scores (64.5 (55.05-75.24); p=0.03). “At-risk” patients were more likely than not “at-risk” patients to report concerns about scar visibility (62% vs 10%), future health problems (40% vs 2%), being treated differently (38% vs 2%), and overprotective parents (33% vs 14%). Eight (57%) of the patients who completed the PeLTQL twice reported a change in PeLTQL-TS exceeding the minimal clinically important difference of 6.45.
Conclusions:
Routine PROM use in pLT surveillance care reveals a disconnect between self- and proxy-reported concerns, with “at-risk” patients more often expressing worries about scar visibility and future health. These findings highlight the need to prioritize the patient voice. A qualitative study exploring coping with surgical scars pLT is underway.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00