Familial Hyperammonemia Requiring Liver Transplantation: A Case Series of Type 1 Citrullinemia
Amala J Alenchery1, Zehra Naseem2, Omar T Sims3, Sobia N Laique4, Kadakkal Radhakrishnan1.
1Department of Pediatric Gastroenterology, Hepatology and Nutrition, Cleveland Clinic Children’s, Cleveland, OH, United States; 2Department of Internal Medicine, Cleveland Clinic, Cleveland, OH, United States; 3Department of Quantitative Health Sciences, Cleveland Clinic Foundation, Cleveland, OH, United States; 4Department of Gastroenterology, Hepatology and Nutrition, Cleveland Clinic Foundation, Cleveland, OH, United States
Background: Symptomatic hyperammonemia is typically associated with liver cirrhosis but may originate from metabolic conditions like urea cycle disorders (UCDs), necessitating a robust diagnostic approach with early decision making regarding liver transplantation (LT). Type 1 citrullinemia is the second most common UCD with limited reports within families.
Methods/Case Description: We describe a case series of four siblings with symptomatic hyperammonemia from type 1 citrullinemia who ultimately underwent orthotopic liver transplantation (LT) at our institution.
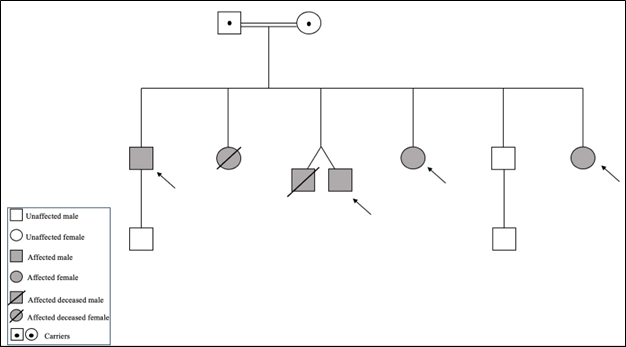
We focus on their age at diagnosis, phenotypic presentation, disease progression despite optimal medical therapy leading to LT, and post-LT course. Patient 1, diagnosed at age 6, developed irreversible learning difficulties and seizures due to multiple hyperammonemia episodes (HAE) which persisted post-LT. Patients 2-4 were diagnosed in the neonatal period with early medical and dietary interventions. They continued to have intermittent HAE and poor growth necessitating LT with ultimate improvement in growth and quality of life.
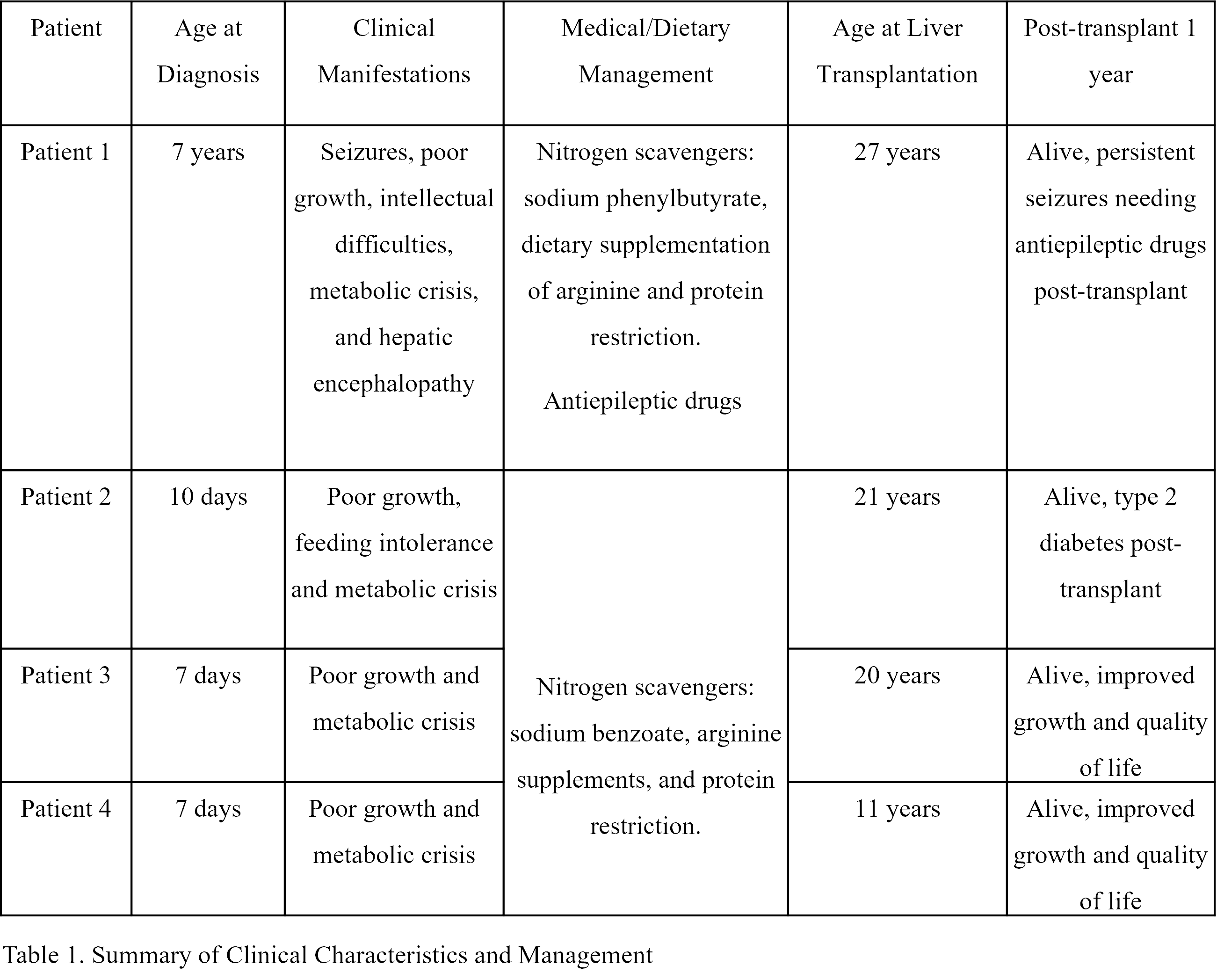
Discussion: UCDs mostly present in the neonatal period, but a high index of suspicion is essential for early diagnosis to improve outcomes. In type 1 citrullinemia, management focuses on medical and dietary therapy to avoid HAE. LT is the only potentially curative option, most effective when performed early for recurrent metabolic issues, failure of medical therapies, or poor healthcare access. Despite LT's comparable survival to medical management, it poses surgical and immunosuppressive risks. Neither strategy can reverse existing neurological damage, underscoring the importance of early diagnosis and a multidisciplinary approach to effectively manage these challenging disorders.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00