A novel strategy to decrease hepatic artery thrombosis in pediatric liver transplantation
Swati Antala1, Kyle Soltys2, Noelle Ebel3, Alex Bondoc4, Bridget Whitehead5, George Mazariegos2, John Bucuvalas1.
1Pediatrics, Icahn School of Medicine at Mount Sinai/RMTI, New York, NY, United States; 2Surgery, UPMC Children's Hospital of Pittsburgh, Pittsburgh, PA, United States; 3Pediatrics, Stanford University, Stanford, CA, United States; 4Pediatric General and Thoracic Surgery, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; 5Pediatrics, Lurie Children's Hospital of Chicago, Chicago, IL, United States
Introduction: Hepatic artery thrombosis (HAT) remains a critical challenge to outcomes after pediatric liver transplantation. We aim to create an actionable approach to decrease HAT incidence using data acquired through the Starzl Network for Excellence in Pediatric Liver Transplantation (SNEPT) to extend the observations of Englesbe et al (AJT 2016) and leverage the variation among centers.
Methods: We retrospectively analyzed pediatric liver transplants from 2017-2022 across 16 SNEPT centers. HAT was defined as vessel occlusion within 30 days of transplant. Primary outcome was the presence or absence of HAT. Chi-square analysis was performed.
Results: 78 HAT were identified among 1624 pediatric liver transplants. 718 (44.2%) transplants were in children < 18 months of age and 906 in children >18 m (55.8%). 50 (64.1%) of the 78 HAT occurred in children < 18 months old compared to 28 in those > 18 months old (p=0.0002). Rates of HAT among centers varied from 0% to 16% and appeared to differ based on total transplant volume. When accounting for variation in center volume, 3 centers emerged with the lowest HAT incidence (Figure 1).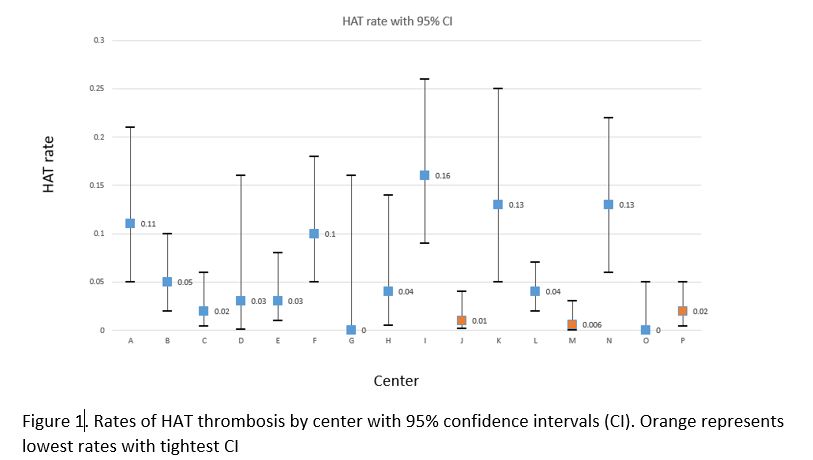
Conclusions: We confirmed that the rate of HAT was significantly higher in children < 18 months of age and identified 3 centers with the lowest incidence of HAT. Transplant volume appeared to influence but not solely define HAT incidence. Analysis is ongoing to explore center-specific perioperative factors driving the variation in HAT incidence among centers. We predict that our findings will inform best practices to improve outcomes.
Starzl Network for Excellence in Pediatric Liver Transplantation (SNEPT) .
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00