Impact of ABO Non-Identical Liver Transplantation on Waitlist Mortality and Post-Transplant Outcomes in Pediatric Candidates
Tess Coker1, Sakil S Kulkarni1, Neeta Vaccharajani2, Janis M Stoll1, Sarah AF Henkel1, William C Chapman2, Darren R Cullinan2, Maria B Doyle2, Adeel S Khan2.
1Department of Pediatrics, Washington University in St Louis, St Louis Children's Hospital., Saint Louis, MO, United States; 2Department of Surgery, Washington University in St Louis, Barnes Jewish Hospital, Saint Louis, MO, United States
Background: Liver transplantation (LT) is crucial for children with end-stage liver disease. Despite improving outcomes, mortality on the waitlist remains critical. Policy permits ABO non-identical LT for high-acuity patients, but the impact in pediatrics is unclear. Understanding blood type distribution is critical for ensuring allocation equity. This study evaluates the influence of ABO non-identical LT on waitlist mortality and post-transplant outcomes in pediatrics.
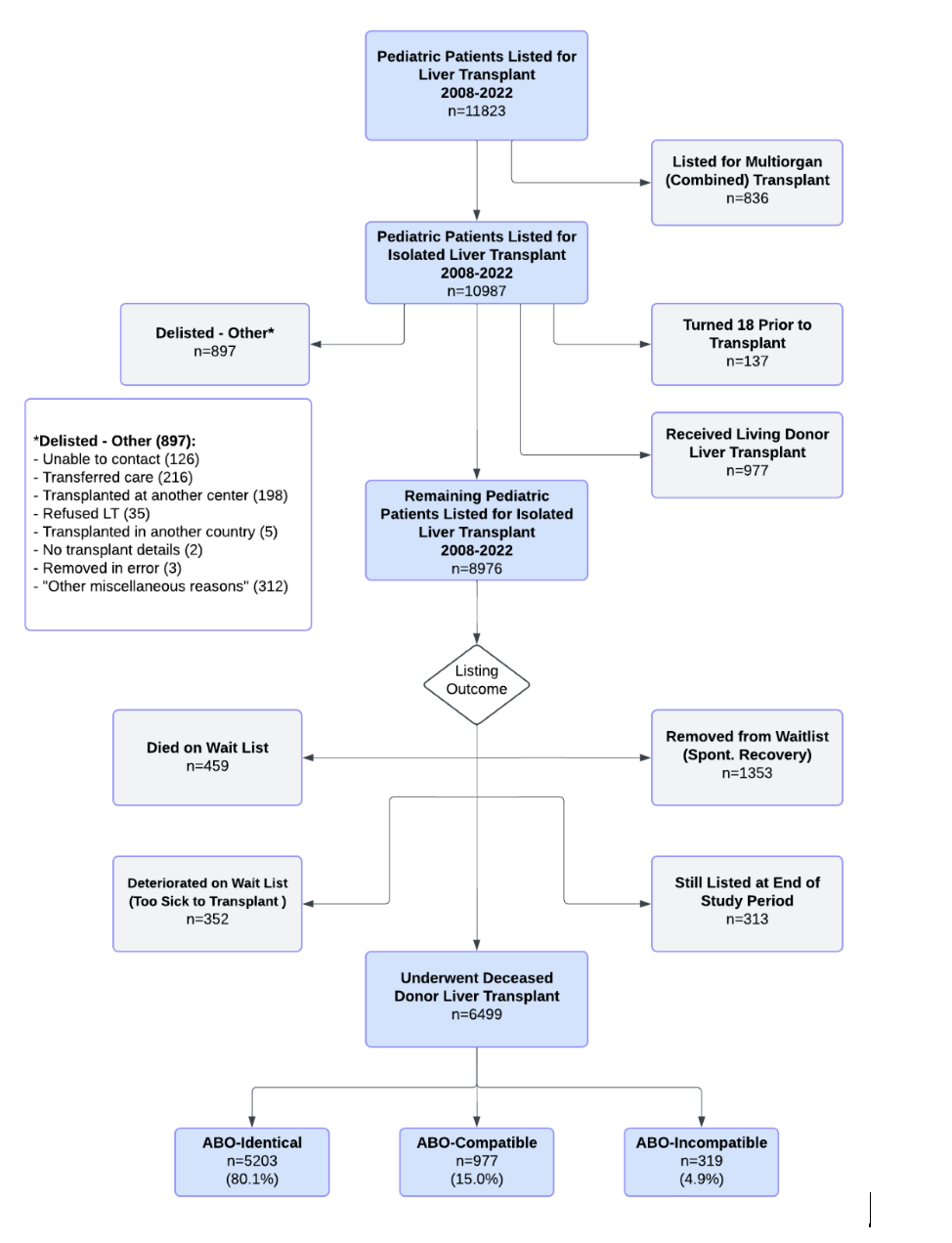
Methods: We retrospectively analyzed the UNOS database for pediatric LT candidates (<18 years) listed for deceased donor liver-only transplant (DDLT) from January 2008 to December 2022. Patients were categorized by blood type and by ABO-identical, ABO-compatible, or ABO-incompatible LT. Specifically, we analyzed the impact of candidate-donor blood matching, including ABO non-identical LT, on outcomes.
Results: 72.4% of 8976 pediatric LT candidates included underwent a DDLT. 19.9% were ABO non-identical, and 4.9% were ABO incompatible. Non-identical LT recipients had significantly higher listing urgency and lower waitlist times. Non-identical LTs led to a net loss of allografts for blood type O, and net gain for all other blood types. Candidates with blood type O had significantly higher waitlist time (62.5 vs. 48 days) and lower proportion of DDLT (70.2% vs. 74.7%) when compared to blood type A.
Conclusion: ABO non-identical allografts result in timely transplant for LT candidates with high acuity. Blood type O candidates are disadvantaged, while blood type A candidates are advantaged. The observations of our study differ from similar adult studies, emphasizing the importance of considering pediatric outcomes.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00