Characterizing caregiver barriers to living donor liver transplantation for pediatric liver transplant recipients: results from the multi-center SOCIAL-Tx study
Morgan Kelly2, Saba Ali1, Andrea Huerta2, Evelyn Hsu3, James E Squires4, Kathleen Campbell7, Nikita Gupta8, Shannon Zielsdorf7, John Bucuvalas5, Jennifer C Lai 2, Sharad I Wadhwani2.
1Pediatrics , University of California, San Francisco , San Francisco , CA, United States; 2Gastroenterology, Hepatology, and Nutrition , University of California, San Francisco , San Francisco , CA, United States; 3Pediatric Gastroenterology and Hepatology , Seattle Children's Hospital, University of Washington , Seattle , WA, United States; 4Pediatric Gastroenterology, Hepatology, and Nutrition , UPMC Children's Hospital of Pittsburgh, University of Pittsburgh , Pittsburgh , PA, United States; 5Pediatric Gastroenterology, Hepatology, and Nutrition , Mount Sinai Kravis Children's Hospital, Ichan School of Medicine at Mount Sinai, New York, NY, United States; 6Pediatric Gastroenterology, Hepatology, and Nutrition , UCSF Benioff Children's Hospital, University of California, San Francisco , San Francisco , CA, United States; 7Transplant Surgery , Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago , IL, United States; 8Pediatric Gastroenterology, Hepatology, and Nutrition , Children's Hospital of Philadelphia, Perelman School of Medicine at the University of Pennsylvania , Philadelphia , PA, United States
SOCIAL-Tx .
Introduction: Living donor liver transplant (LDLT) mitigates organ shortages and is associated with superior patient and graft survival. Only 17% of pediatric liver transplants involve living donors; these rates are lower among socioeconomically deprived children. We characterized qualitative barriers and facilitators to LDLT among families reporting household social risks (e.g., food insecurity) across 6 transplant centers.
Methods: We conducted one-hour in-depth interviews with caregivers of children who underwent liver transplant and enrolled in the SOCIAL-Tx study. Interviews were recorded and professionally transcribed. Two reviewers independently coded transcripts using a codebook informed by the COM-B model, an implementation science framework. Codes were compared and reconciled to generate themes.
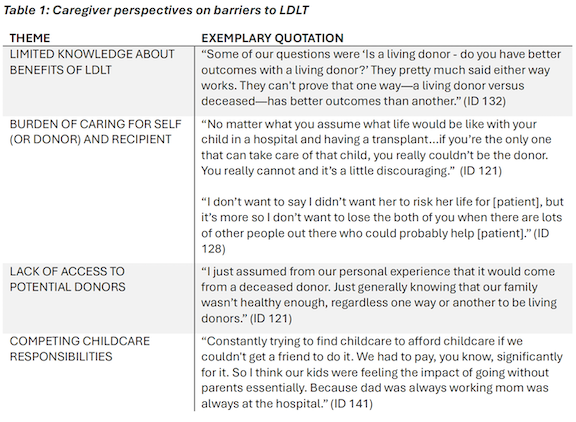
Results: Fifteen caregivers participated; 50% reported household incomes below 150% of the federal poverty level, 80% were female, 60% were White, 27% were Hispanic, 6.5% Black, and 6.5% were Asian/Pacific Islander. Four themes emerged: (1) limited knowledge about the benefits of LDLT, (2) concern about caring for both the donor and recipient, (3) perceived lack of access to living donors, and (4) competing childcare responsibilities (Table 1).
Conclusion: No caregivers opposed LDLT for their child. Interventions that increase awareness of the benefits of LDLT early in the evaluation process, connect families to non-directed donors, and support caregivers find resources for childcare throughout the transplant journey may improve uptake of LDLT. Such efforts should prioritize under-resourced families to enhance equitable access and outcomes for pediatric liver transplant recipients.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00