Immediate and Early Extubation After Pediatric Liver Transplantation: A retrospective cohort study
Doaa Fahmy1,2, Mohammad Maudarbaccus3, Elaine Gilfoyle4, Vicky Ng1, Blayne Sayed5,6,7, Asad Siddiqui8.
1Division of Gastroenterology, Hepatology, and Nutrition, The Hospital for Sick Children, Toronto, ON, Canada; 2Division of Gastroenterology, Hepatology and Nutrition, Mansoura University Children’s Hospital, Mansoura, Egypt; 3Department of Intensive Care Medicine and Anesthesia, The Beacon Hospital, Dublin,, Ireland; 4Department of Critical Care, The Hospital for Sick Children, Toronto, ON, Canada; 5Division of General and Thoracic Surgery, The Hospital for Sick Children, Toronto, ON, Canada; 6Transplant and Regenerative Medicine Center, The Hospital for Sick Children, Toronto, ON, Canada; 7Ajmera Transplant Center, University Health Network, Toronto, ON, Canada; 8Department of Anesthesia and Pain Medicine, The Hospital for Sick Children, Toronto, Toronto, ON, Canada
Pediatric liver transplantation recipients .
Introduction: Prolonged mechanical ventilation after liver transplantation (LT) is associated with deleterious clinical outcomes. Intraoperative extubation (IE) and early extubation (EE) became more prevalent in literature. The purpose of this study is to investigate rates, outcomes and predictors of IE and EE at a single high-frequency pediatric transplant center.
Method: Perioperative data of patients aged <18 years with isolated LT between January 1, 2013, to January 10, 2022, was retrospectively reviewed. Patients were divided into 3 groups; IE, EE ≤ 24h and delayed extubation >24h (DE). The primary outcome was development of pulmonary complications while secondary outcomes included ventilator associated pneumonia, reintubation, reoperation, graft complications, ICU and hospital length of stay (LOS). Multivariable logistic regression was conducted to identify predictors of IE and EE, compared to DE.
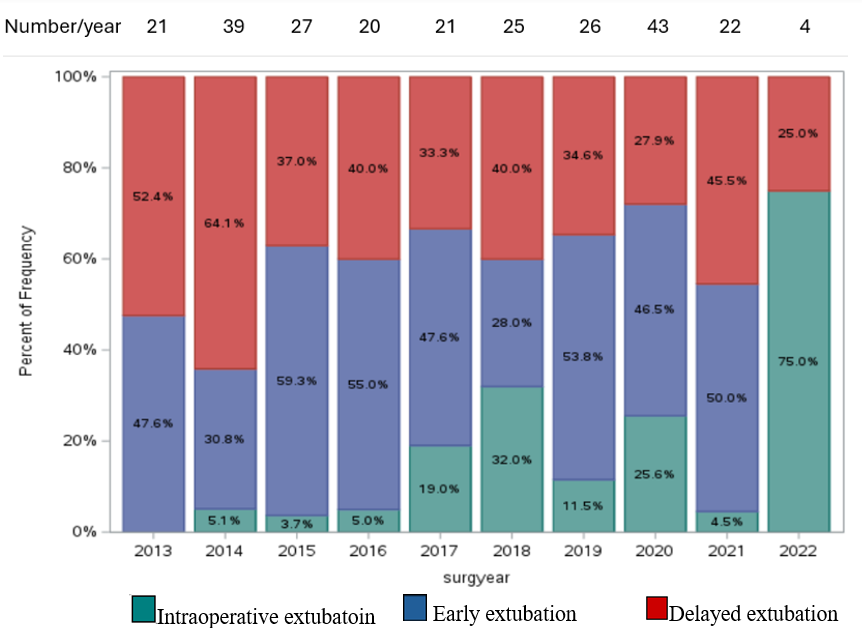
Results: Of 248 patients, 34 and 111 had IE and EE respectively. There was a rising trend of IE and EE rates during the study period (Figure 1). There were statistically significant differences among the 3 groups in both primary and secondary outcomes (p-value <0.001), confirming that longer duration of mechanical ventilation was associated with higher rates of complications. Only age, regional block and packed red blood cell pRBC transfusion were selected as good predictors of successful IE/EE, with p-value of 0.001, 0.013, 0.002 respectively and AUC at 0.79.
Conclusion: IE and EE after pediatric LT became more common at our institution. It is a safe approach with favorable postoperative outcomes. Age, regional block and intraoperative pRBC can predict successful IE and EE.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00