One-year outcomes of a liver transplant paired exchange for two pediatric recipients
Kathryn LaRusso1, Piyush Gupta1, Juan Francisco Guerra1, Khalid Khan2, Udeme Ekong2, Pejman Radkani1, Alexander Kroemer1, Nada Yazigi2, Gabriel Gondolesi1, Cal Matsumoto1, Thomas Fishbein1.
1Georgetown Transplant Institute, MedStar Georgetown University Hospital, Washington, DC, United States; 2Pediatric Transplant Hepatology, Georgetown Transplant Institute, MedStar Georgetown University Hospital, Washington, DC, United States
Introduction: Liver paired exchange (LPE) is a method to reduce donor ineligibility when blood type or size mismatches occur between a donor and recipient. Prior reports of LPE from North America have only highlighted transplants between adult recipients or a combination of adult and pediatric recipients. Here we present a successful case of LPE for two pediatric recipients with one-year outcomes.
Methods: A retrospective chart review was conducted aiming to present our initial experience with a pediatric LPE.
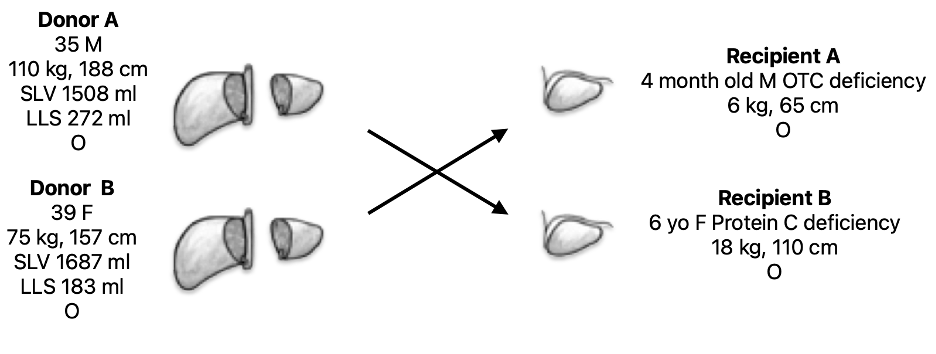
Results: The paired exchange occurred September 2023 and included a 35-year-old male with to an unrelated 6-year-old female diagnosed with protein C deficiency. The second pair was an altruistic 39-year-old female to a four-month-old male with ornithine transcarbamylase deficiency (OTC), related to the first male donor. All patients were blood type O. Both infants received a left lateral segment graft with conventional anatomy. The LPE allowed for a more appropriate graft-to-recipient weight ratio (GRWR) for the infant recipient, 2.6% versus 4.2%, for a directed donation. The other child’s GRWR was well matched at 1.6% with the swap. Neither of the donors had complications and were doing well at 1-year follow-up. Both recipients returned to the operating room initially for complete and partial hepatic artery thrombosis requiring revision. One had a subsequent bile leak requiring biliary drainage. Both grafts were salvaged, and both recipients are alive with functional grafts at 16 months post-operatively.
Conclusion: Liver paired exchange between two pediatric recipients can reduce size incompatibilities and one-year outcomes support continued programmatic growth. Early identification and treatment of complications can also reduce graft loss.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00