Living donor liver transplantation in a pediatric patient with situs inversus: case report and systematic review
Nadia F. Ali BS1, Piyush Gupta MD2, Kathryn LaRusso MD, PhD2, Nada Yazigi MD2, Carolina Rumbo MD2, Christof Kaltenmeier MD2, Juan Guerra MD2, Udeme Ekong MD2, Alexander Kroemer MD, PhD2, Khalid Khan MD2, Cal Matsumoto MD2, Thomas Fishbein MD2, Gabriel Gondolesi MD2.
1Georgetown University School of Medicine, Washington, DC, United States; 2Medstar-Georgetown Intestinal Care and Transplant Center, Georgetown University, Washington, DC, United States
Introduction: Liver transplantation (LT) with situs inversus (SI) is a rare and challenging procedure. Current literature is limited. We here report a video presentation on the technical aspects and outcomes of a pediatric recipient with SI abdominalis who underwent LT for biliary atresia.
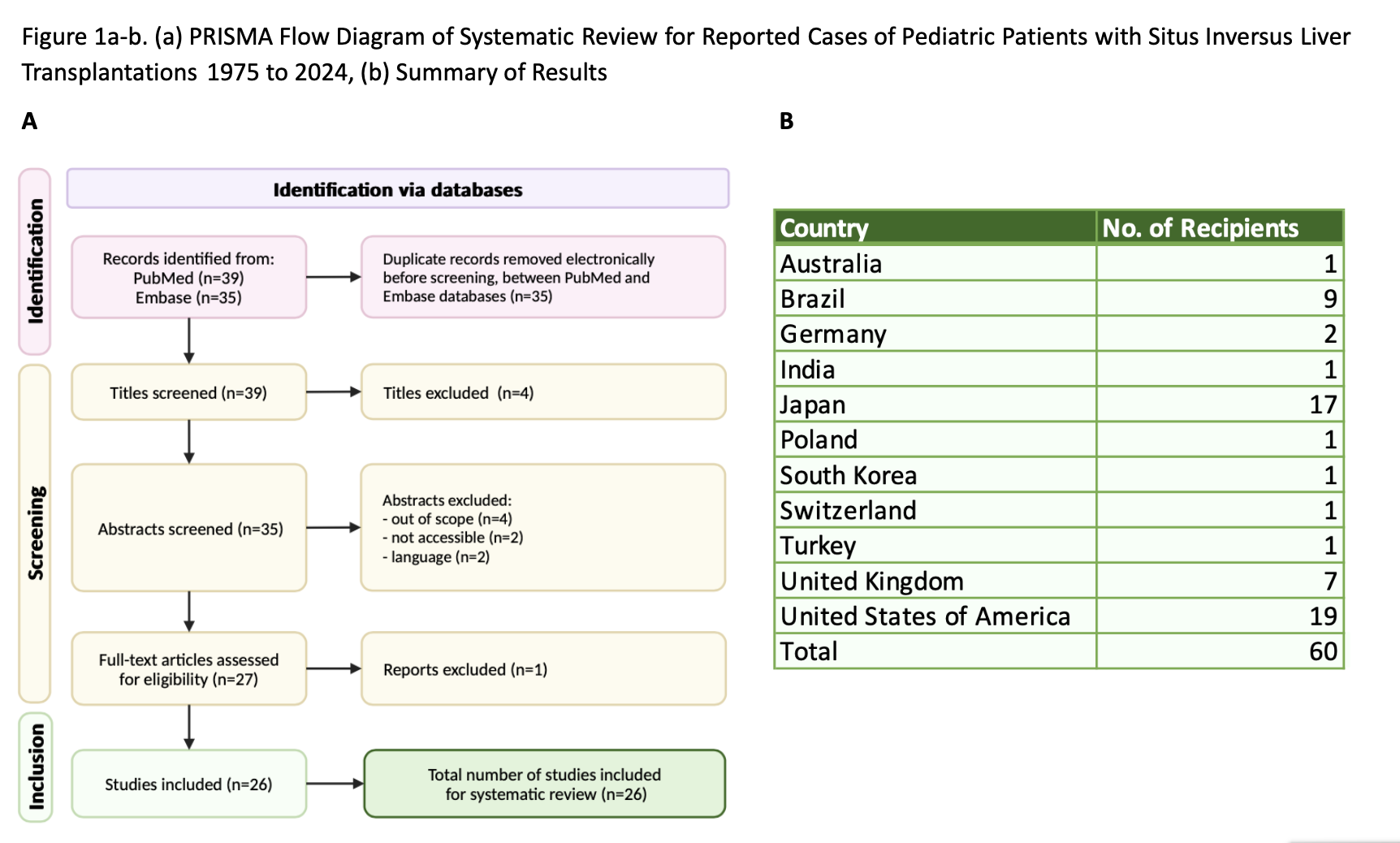
Patient and Methods: A 6-month-old female weighing 8 kg with an uncomplicated birth history developed cholestasis at 10 days of life. Imaging revealed SI abdominalis, biliary atresia, polysplenia, levocardia, and absence of inferior vena cava. Subsequently, she underwent exploratory laparotomy with a Kasai procedure and Meckel's diverticulectomy. The Kasai failed, leading to decompensated liver disease. She then underwent living-donor left-lateral lobe LT. In addition, a systematic review of the literature was conducted: flow diagram in Figure 1a.
Results: This complex procedure required an extension graft of the left hepatic vein from a cadaveric inferior cava that was connected to the common orifice of the 3 hepatic veins. The portal veins were anastomosed using a cuff of the left and right portal veins to the donor left portal vein. Arterial inflow was reconstructed between the donor and recipient proper hepatic arteries. Bile duct reconstruction was done by utilizing the previous Roux-en-Y Hepatico-jejunostomy but required creating 2 separate anastomoses. She evolved without complications and was discharged 12 days after the procedure. Systematic review results are summarized in Figure 1b.
Conclusion: Rare congenital abnormalities such as SI should not be considered a contraindication for LT. We provide an example of a successful case to add to the existing literature.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00