Pediatric liver transplantation for metabolic diseases, the Georgetown experience.
Nada Yazigi MD1, khalid Khan MD1, Alexander Kroemer MD1, Udeme Ekong MD1, Juan F guerra MD1, Brian Nguyen MD1, Carolina Rumbo MD1, Pejman Radkani MD1, Megan Johnson PA-C1, Megan Song BSN1, Chelsea Sooy BSN1, Kathryn Larusso MD1, Lindsey Beldsoe PA-C1, Christopher kaltenmier MD1, David Walls MD1, Tammy Hanel RD1, Erica W Chen1, Maeen Arsalan1, michelle Eaton RN1, Julia Clayton RN1, Megha Fitzpartick MD1, Gabriel Hauser MD1, kimberly Chapman MD2, Debra Regier MD2, nicholas ahMew MD2, Cal Matsumoto MD1, Gabriel Gondolesi MD1, Tom Fishbien MD1, Stuart kaufman MD1.
1Medstar Transplant Institute , Medstar georgtown university hosptial, Washington DC, DC, United States; 2Rare Diseases Institute, Children National medical center, Washington DC, DC, United States
Liver transplantation (LT) is a well-established treatment for pediatric patients with metabolic liver diseases (MLDs) unresponsive to medical management. MLDs account for approximately 15% of pediatric LT indications. The most common MLDs leading to LT include urea cycle disorders (UCD), organic acidemias (MSUD, MMA, PA,), and glycogen storage diseases (GSD). In these conditions, LT not only restores normal liver function but also corrects or palliate the underlying metabolic defect by providing a source of the deficient enzyme.
Material and methods: The following variables were extracted from medical records of patients receiving a LT for a MLD between 1/2003 and 1/2024: type of MLD, wait-time for LT, age at LT, type of LT, length of post-op total hospital and PICU stay, and patient/graft survival. Patients lost to follow-up and those re-transplanted were excluded. The study was conducted under the IRB #2017-0365. Analysis was done using SPSSÒ v.29.0.02.
Results: 109/353 (31%) pediatric LT performed at our institution were for MLDs including: UCD: 30, MSUD: 21, PFICs’: 14, PA: 11, MMA: 8, a1-AT: 4, GSD: 5, others:16. The mean age at LT 4.27 ± 5.09 years, mean time on the waiting list: 126.4 ± 168.4 days; the analysis of the most frequent MLDs’ results are shown in table 1. Sixty-three (58%) received whole organs, 21 (19%) Splits, 18 Living donors (16%) and 7 reduce grafts. Three patients died (2.7%), and other 4 grafts were lost. The overall Patient survival was: 99% 1st year, 98% at 3rd and 5th years, while Graft survival was: 95% 1st year, 95% 3rd year and 94% 5th year. Patient and Graft survival analysis by primary disease and graft types were not different among the prevalent diseases.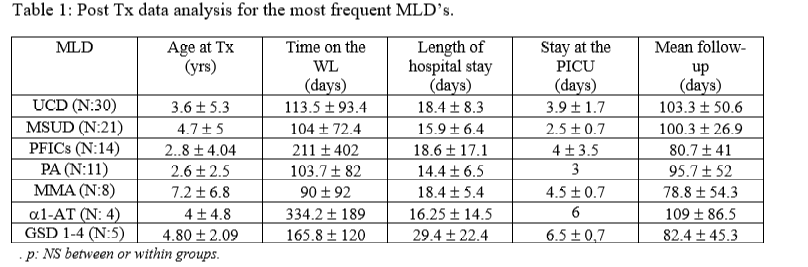
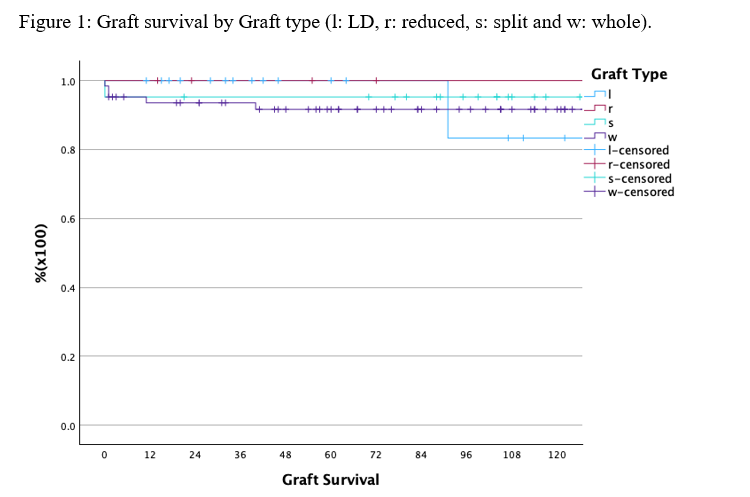
In conclusion, LT offers a life-saving intervention for pediatric patients with MLDs, providing excellent short- and long-term outcomes. Graft type does not impact on survival. A multidisciplinary approach is crucial to address the complex needs of these patients and to ensure optimal results.
The WebApp is sponsored by:

If you have any questions during the meeting, please go to the registration desk. Our emails will be monitored sporadically.
REGISTRATION DESK OPENING TIMES
Thursday, May 1, 2025, 07:00-17:30 Friday, May 2, 2025, 07:00-12:00